
2MG
This product is for research purposes only. Not for human consumption.
Purity: >98% (HPLC verified)
Formulation: Lyophilized powder
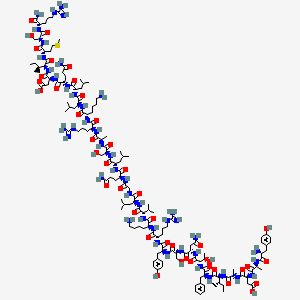
Molecular Formula: C149H246N44O42S
Molecular Weight: 3357.96 g/mol
CAS Number: 86168-78-7
PubChem CID: 16132413
Sermorelin
Overview
Sermorelin (GRF 1-29 NH2 or Growth Hormone-Releasing Factor 1-29 amide) is a synthetic peptide consisting of the first 29 amino acids of the full 44-amino acid human growth hormone-releasing hormone (GHRH, also known as growth hormone-releasing factor or GRF) that is naturally produced by neurons in the arcuate nucleus of the hypothalamus and released into the hypophyseal portal circulation to stimulate growth hormone secretion from the anterior pituitary.
Development and FDA Approval
The development of Sermorelin arose from research in the 1970s-1980s that characterized GHRH structure, function, and identified that the biologically active portion responsible for GH-releasing activity resides in the N-terminal region of the molecule, specifically amino acids 1-29, while the C-terminal portion (amino acids 30-44) is not required for receptor binding or signaling. This discovery enabled the creation of a shorter, synthetically producible peptide that retains full biological activity while being more practical and cost-effective to manufacture than the full-length 44-amino acid hormone.
Sermorelin received FDA approval in 1997 for diagnostic testing of growth hormone secretory capacity in children and adults (evaluating pituitary function and reserve), though this approval has since been discontinued and Sermorelin is now available primarily through compounding pharmacies for off-label use in growth hormone deficiency and anti-aging applications.
Advantages Over Direct GH Administration
The rationale for using Sermorelin rather than direct growth hormone (GH) administration is based on several key advantages of working through the body's endogenous hormone system: Sermorelin stimulates pulsatile GH release that mimics natural physiological secretion patterns, with GH levels rising and falling in accordance with the body's circadian rhythms and metabolic needs, whereas exogenous GH provides constant supraphysiological levels that can override normal regulation.
Pulsatile GH patterns are important for optimal receptor sensitivity and metabolic effects - continuous GH exposure can lead to receptor downregulation and may have different metabolic consequences than pulsatile patterns. Sermorelin stimulation preserves negative feedback loops mediated by IGF-1, somatostatin, and other factors, creating a self-limiting system that helps prevent excessive GH production and associated risks like acromegaly-like symptoms, severe insulin resistance, or fluid retention.
By working through the hypothalamic-pituitary axis, Sermorelin also maintains the body's ability to modulate GH secretion based on physiological needs - for example, endogenous GH release is increased during deep sleep, exercise, and fasting, and Sermorelin stimulation respects these natural rhythms. Additionally, Sermorelin's effects decline when pituitary capacity is exhausted or inhibitory signals (somatostatin) are active, providing intrinsic safety compared to pharmacological GH administration.
Applications and Administration
These properties make Sermorelin attractive for addressing age-related GH decline (which affects body composition, energy, sleep, cognitive function, and overall vitality in many aging individuals), optimizing GH levels in athletes and fitness enthusiasts seeking performance and recovery benefits, and potentially treating growth hormone deficiency states where restoring pituitary function is preferable to GH replacement.
However, it's important to note that Sermorelin is only effective when the pituitary gland retains functional capacity to produce GH - in cases of severe pituitary damage, tumor, or congenital absence of somatotrophs, direct GH replacement would be required as Sermorelin would have no tissue to stimulate. The peptide is typically administered via subcutaneous injection, commonly before bedtime to augment the natural nocturnal GH pulse, at doses ranging from 100-500 mcg or more depending on indication and individual response.
Mechanism of Action
Sermorelin exerts its effects through high-affinity binding to and activation of growth hormone-releasing hormone receptors (GHRHR) expressed on somatotroph cells in the anterior pituitary gland. These somatotrophs constitute approximately 50% of the anterior pituitary cell population and are specialized for synthesis and secretion of growth hormone (GH, also called somatotropin), a 191-amino acid peptide hormone that is one of the most important regulators of growth, metabolism, and body composition.
Receptor Mechanism and Signaling
GHRHR is a member of the class B family of G-protein coupled receptors (GPCRs), characterized by a large extracellular N-terminal domain that binds peptide ligands. When Sermorelin binds to GHRHR, it causes a conformational change that activates coupled Gs proteins, which stimulate adenylyl cyclase to catalyze conversion of ATP to cyclic AMP (cAMP).
Elevated intracellular cAMP levels activate protein kinase A (PKA), which phosphorylates multiple downstream targets including transcription factors like CREB (cAMP response element-binding protein). Phosphorylated CREB translocates to the nucleus where it binds to cAMP response elements (CREs) in DNA, upregulating transcription of the growth hormone gene and other genes involved in GH synthesis and secretion.
GH Release and Regulation
This transcriptional activation increases GH mRNA and protein synthesis over hours to days with sustained Sermorelin stimulation. Additionally, cAMP/PKA signaling rapidly mobilizes GH-containing secretory granules and promotes their fusion with the plasma membrane, causing acute release of stored GH into the hypophyseal capillaries that drain into systemic circulation.
The time course of GH release after Sermorelin administration typically shows peak GH levels occurring 15-60 minutes after injection, with levels declining over the following hours as the peptide is cleared and inhibitory mechanisms (particularly somatostatin release) engage.
Negative Feedback Regulation
Importantly, Sermorelin stimulation is subject to physiological regulation through the somatostatin-GHRH axis: when GH and IGF-1 levels rise, this triggers negative feedback at the hypothalamus, stimulating release of somatostatin (also called growth hormone-inhibiting hormone or GHIH) from periventricular hypothalamic neurons.
Somatostatin binds to somatostatin receptors on somatotrophs, which couple to Gi proteins that inhibit adenylyl cyclase, reduce cAMP levels, and suppress both GH synthesis and release - directly opposing Sermorelin's stimulatory effects. This negative feedback creates self-limiting GH stimulation that helps prevent dangerous overproduction.
Timing and Circadian Effects
The pituitary also has intrinsic rhythmicity and responsiveness that varies throughout the day and in different metabolic states - somatotrophs are more responsive to GHRH stimulation during certain circadian phases (particularly during sleep), after exercise, during fasting, and in the presence of ghrelin (the "hunger hormone" that synergizes with GHRH to amplify GH release).
This explains why Sermorelin timing matters - evening administration before sleep aligns with natural nocturnal GH surges, while daytime administration might be attenuated by higher ambient somatostatin tone.
Downstream GH Effects
Once GH is released into circulation, it exerts diverse physiological effects through multiple mechanisms. GH directly binds to growth hormone receptors (GHR) expressed in virtually all tissues, triggering JAK-STAT signaling pathways, MAPK cascades, and other intracellular signals that regulate gene transcription, protein synthesis, lipolysis, and other metabolic processes.
Many of GH's growth-promoting and anabolic effects are mediated indirectly through stimulation of insulin-like growth factor-1 (IGF-1) production, primarily in the liver but also in peripheral tissues. Circulating and local IGF-1 then binds to IGF-1 receptors to promote protein synthesis, cell proliferation, tissue growth, and metabolic regulation.
The GH/IGF-1 axis promotes muscle protein synthesis and lean body mass gain, enhances lipolysis and fat oxidation (reducing adipose tissue), stimulates bone formation and mineralization, supports immune function, influences cognitive function and mood, improves sleep quality and architecture, enhances skin collagen production and thickness, and modulates glucose and lipid metabolism.
Aging is associated with progressive decline in GH and IGF-1 levels - by age 60, many individuals have GH secretion that is 50-70% lower than peak young adult levels, a phenomenon sometimes called somatopause. Sermorelin aims to partially restore more youthful GH levels and pulsatility.
Research Findings
Research on Sermorelin encompasses several decades of investigation ranging from initial characterization of GHRH and development of synthetic analogs, through clinical trials for growth hormone deficiency diagnosis and treatment, to more recent exploration of anti-aging and performance enhancement applications.
Foundational Research
The foundational work in the 1980s by researchers including Guillemin, Rivier, and others established that synthetic GRF(1-29)-NH2 (Sermorelin) possesses full biological activity for stimulating GH release equivalent to the full 44-amino acid GHRH, validating the concept that only the N-terminal 29 amino acids are required for receptor binding and activation.
Early pharmacological studies characterized Sermorelin's dose-response relationships, showing that doses as low as 1 mcg/kg can stimulate significant GH release, with maximal responses typically achieved at doses of 1-3 mcg/kg in diagnostic testing contexts.
Pediatric Studies
Clinical studies in children with growth hormone deficiency demonstrated that chronic Sermorelin administration (typically 30 mcg/kg given subcutaneously three times per week or daily before bedtime) could stimulate growth velocity, increase height percentile, and improve growth outcomes, though direct GH replacement generally produced more robust growth than GHRH analog therapy and became the standard treatment for pediatric GH deficiency.
However, Sermorelin offered theoretical advantages including preservation of pulsatile GH patterns, potential for improved safety, and possible enhancement of endogenous pituitary function rather than suppression.
Adult Growth Hormone Deficiency
Adult growth hormone deficiency research explored Sermorelin as an alternative to GH replacement therapy. Studies showed that Sermorelin treatment in adults with GHD could increase IGF-1 levels, though not always to the same extent as GH replacement, and produce improvements in body composition (increased lean mass, reduced fat mass), energy levels, exercise capacity, and quality of life measures.
However, response variability was noted, with better outcomes in individuals with preserved pituitary function and less severe GHD.
Age-Related Decline Research
Age-related GH decline research has investigated Sermorelin for treating somatopause. Studies in healthy elderly individuals showed that Sermorelin administration could increase GH and IGF-1 levels toward more youthful ranges, with associated improvements in body composition (increased lean mass, reduced abdominal adiposity), sleep quality (enhanced slow-wave sleep), skin thickness, bone density markers, and subjective energy and vitality.
A notable study published in JAMA examined effects of 6 months of GHRH administration in healthy elderly men, showing significant increases in lean body mass and reductions in adipose tissue. However, the magnitude of benefits has been debated, with some studies showing modest effects and questions about clinical significance.
Combination Therapy and Athletic Applications
Combination therapy research has explored Sermorelin together with growth hormone-releasing peptides (GHRPs) like GHRP-2, GHRP-6, or Ipamorelin, based on the concept that GHRH and GHRPs work through complementary mechanisms (GHRHR versus ghrelin receptor pathways) and can produce synergistic GH release when combined - indeed, clinical data supports enhanced GH stimulation with combination therapy versus either agent alone. Some protocols pair Sermorelin with Ipamorelin for optimized GH stimulation.
Athletic performance and body composition research in physically active individuals has shown that Sermorelin, particularly when combined with resistance training, can enhance lean mass gains, reduce body fat, improve recovery, and support performance, though rigorous controlled trials in athletic populations are limited.
Sleep and Safety Studies
Sleep research has documented that GHRH administration can enhance slow-wave (deep) sleep, the most restorative sleep stage that naturally coincides with GH secretory pulses. Sermorelin given before bedtime may improve sleep architecture, which has benefits for recovery, cognition, and overall health.
Safety and tolerability studies have generally found Sermorelin well-tolerated with fewer adverse effects than direct GH therapy, though injection site reactions, flushing, headache, and occasional dizziness can occur.
Research Applications
- Age-related growth hormone decline and somatopause research
- Growth hormone deficiency diagnosis and treatment studies
- Anti-aging and longevity medicine research
- Body composition optimization (lean mass, fat reduction) studies
- Sleep quality and slow-wave sleep enhancement research
- Athletic performance, recovery, and training adaptation research
- Metabolic health and insulin sensitivity studies
- Bone health and osteoporosis prevention research
- Pituitary function assessment and testing
- Combination therapy with GHRPs research
- Skin health, collagen synthesis, and aesthetic medicine studies
- Cognitive function and mood in aging research
- Immune function and immunosenescence studies
- Cardiovascular health and exercise capacity research
Safety Profile
Sermorelin has demonstrated a generally favorable safety profile across clinical studies and extensive off-label use, with fewer and less severe adverse effects compared to direct growth hormone therapy, primarily because it works through physiological stimulation of endogenous GH production with intact regulatory feedback mechanisms rather than providing pharmacological doses of exogenous hormone. The most commonly reported side effects are mild and include injection site reactions (redness, pain, swelling) at subcutaneous administration sites, typically transient and manageable with proper injection technique and site rotation. Flushing or warmth, particularly in the face and upper body, can occur shortly after injection in some individuals, related to vasodilatory effects and usually resolving within minutes. Headache is reported by some users, typically mild and decreasing with continued use. Dizziness or lightheadedness occasionally occurs, possibly related to transient changes in blood pressure or glucose. Nausea is uncommon but can occur, especially with higher doses. Some individuals report hyperactivity, restlessness, or difficulty sleeping if Sermorelin is administered too late in the evening or if they are particularly sensitive to GH's stimulatory effects, though many users conversely report improved sleep quality, particularly enhanced deep sleep. Unlike direct GH therapy, Sermorelin rarely causes significant fluid retention, carpal tunnel syndrome, joint pain, or severe insulin resistance that can complicate GH replacement, though mild versions of these effects are theoretically possible if GH stimulation is excessive. Glucose metabolism effects are generally milder than with GH therapy, but individuals with diabetes or prediabetes should monitor blood glucose as GH can increase insulin resistance and blood sugar levels. Contraindications include active malignancy (GH/IGF-1 could theoretically promote tumor growth, though evidence is mixed), hypersensitivity to Sermorelin or GHRH, pituitary tumors or masses (stimulation could theoretically promote growth), and pregnancy/lactation (safety not established). Individuals with hypothyroidism should have thyroid function optimized before starting Sermorelin as GH can affect thyroid hormone metabolism and requirements. Long-term safety data is less extensive than for GH, but years of clinical use have not revealed major safety concerns. Antibody formation against Sermorelin can theoretically occur with chronic use, potentially reducing efficacy, though clinical significance appears limited. Unlike GH, Sermorelin is unlikely to cause acromegaly-like features, severe metabolic derangements, or pituitary suppression because endogenous regulatory mechanisms remain active. Sermorelin use in athletes is prohibited by most sports organizations as a performance-enhancing substance. Overall, with appropriate patient selection, dosing, and monitoring (periodic IGF-1 testing, glucose monitoring in at-risk individuals, clinical assessment), Sermorelin appears to have a favorable benefit-to-risk profile for addressing GH deficiency or age-related GH decline.
Scientific References
Research Use Only
This product is intended for research purposes only and is not for human consumption, therapeutic use, or diagnostic applications. Please ensure compliance with all applicable regulations and institutional guidelines.